What causes pain in the heel?
Pain in the heel can be caused by many things. The commonest cause is plantar fasciitis. Other causes include:
- being overweight
- constantly being on your feet, especially on a hard surface like concrete and wearing hard-soled footwear
- thinning or weakness of the fat pads of the heel
- arthritis in the ankle or heel (subtalar) joint
- irritation of the nerves on the inner or outer sides of the heel
- fracture of the heel bone (calcaneum)
What is plantar fasciitis?
The function of the heel in walking is to absorb the shock of your foot striking the ground and to start springing you forward on the next step. The heel bone, or calcaneum, is cushioned by specialised fat, contained in elastic pockets, within the thickened skin of the heel. It contains a strong bone (the calcaneum).
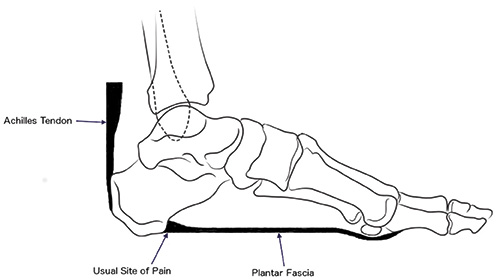
There are a number of strong ligaments, which run between the calcaneum and the toes. Amongst other things this ligament helps support the arch of the foot. The strongest of these ligaments is the plantar fascia. The plantar fascia takes a lot of stress as you walk, or even just standing.
In some people the plantar fascia becomes painful and inflamed. This usually happens where it is attached to the heel bone, although sometimes it happens in the mid-part of the foot. This condition is called plantar fasciitis.
Causes include:
- Constant stress. Plantar fasciitis is therefore commoner in people who spend all day on their feet, or are overweight.
- Stiffness of the ankle or tightness of the Achilles tendon increase the stresses on the heel. Most people with plantar fasciitis have a rather tight Achilles tendon.
- People who have high-arched (‘cavus’) feet or flat feet are less able to absorb the stress of walking and are at risk of plantar fasciitis
- Occasionally plantar fasciitis starts after an injury to the heel.
- People who have a rheumatic condition such as rheumatoid arthritis or ankylosing spondylitis may get inflammation anywhere a ligament is attached to bone (enthesopathy), and plantar fasciitis in these people is part of their general condition.
Usually plantar fasciitis eventually gets better itself, but this can take months or even years. If you have it once you are more likely to get it again.
I’ve been told my pain is caused by a bone spur. Is this likely?
Near the inflamed plantar fascia attachment, but not in it, some extra bone may form, producing a small ‘spur’. In fact, it is a shelf of bone, not a sharp spur. These ‘heel spurs’ are commoner in people with plantar fasciitis, but they can be found in people with no heel pain. The heel spur is caused by the same process as the heel pain, but the spur is not itself the cause of the pain.
Can I do anything about heel pain myself?
You can try to avoid the things that cause heel pain to start:
- Lose weight
- Where your job allows, minimise the shock to your feet from constant pounding on hard surfaces, both by reducing the time you spend on your feet, and wearing shoes with a soft, cushioned heel (such as training shoes).
- Reduce the shocks on your heel by choosing footwear with some padding or shock-absorbing material in the heel. Heel pads can be bought in most chemists. These pads can be put in standard shoes to reduce the impact of walking.
- If you have an injury to your ankle or foot, make sure you exercise afterwards to get back as much movement as possible to reduce the stresses on your foot and your heel in particular
If you start to get heel pain, doing the above things may enable the natural healing process to get underway and the pain to improve.
When should I take professional advice?
If your heel pain is affecting your normal activities and not getting better with simple self-treatment you may wish to consult your GP. (You may prefer to put up with it, knowing it will probably get better eventually.)
How will my doctor tell what is wrong?
Your doctor will listen to your complaints about your heel and examine you to see what is causing the pain, and whether anything else has started it off. If the cause of your pain seems obvious, your doctor may be happy to start treatment straight away.
However, some tests may be helpful in ruling out other problems. Blood tests may be done for arthritis. An X-ray will show any arthritis in the ankle or subtalar joint, as well as any fracture or cyst in the calcaneum. (It will also show a spur if you have one, but as we know this is not the cause of the pain.) Occasionally a bone scan may be used to help spot arthritis or a stress fracture.
What can be done about heel pain?
As heel pain is basically a stress problem in the tissues of the heel, the main treatment is to reduce stress.
Self help:
- Your doctor will advise you about weight-loss and appropriate footwear.
- A soft heel pad is useful to wear in your shoe to act as a shock-absorber when you walk.
- If you have a stiff ankle or tight Achilles tendon simple exercises can be used to stretch the heel cord. Stretching the Achilles tendon and plantar fascia is very effective general treatment for many patients, however it is important that you undertake the exercises regularly.
- Lean your arms against a solid and secure table
- Put one leg behind the other as shown.
- By bending the front knee, and keeping the back knee straight (arrow) you should feel the calf muscles (star) get tight.
- Hold this position for 30 seconds (timed). Do not rock back and forth.
- Change your legs over, so that you stretch the opposite calf. Plantar fasciitis can affect both legs, and so stretch both legs.
- Perform the exercise on both legs twice – the whole exercise takes 2 minutes.
- Repeat the exercise 4 times per day.
Simple pain-killers such as paracetamol or anti-inflammatory medicines ( for example Brufen, Nurofen) can help reduce the pain. Ask advice from your doctor or pharmacist before taking anti-inflammatory medicines as they can have troublesome side-effects in some people.
The simple measures above will help the majority of people with heel pain. In fact after about one year 95% of people’s symptoms settle. It is improtant to be patient, and stick to the treatment programme.
If the pain continues, specialist treatment may be required. There are numerous options, these include:
- Wearing a splint at night to stretch your Achilles’ tendon, while you are asleep
- Injection of steroid (an anti-inflammatory agent) into the attachment of the plantar fascia to damp down the inflammation.
These measures will reduce the pain in most people who are not helped by simple treatment. If you still have pain after one or two injections, your doctor may want to investigate your problem a bit further. If no other medical problem or cause of stress in your heel is found, a number of other treatments can be tried:
- Further physiotherapy
- Resting the foot in a plaster cast to rest the inflamed tissues
- Shock wave treatment
Only if all non-surgical treatments fail would an operation be considered – this is because surgery has risks attached to it, and is not always successful.
Do I need an operation?
It is rare to need an operation for heel pain. It would only be offered if all simpler treatments have failed and, in particular, you are a reasonable weight for your height and the stresses on your heel cannot be improved by modifying your activities or footwear.
The aiThe aim of an operation is to release part of the plantar fascia from the heel bone and reduce the tension in it. Many surgeons would also explore and free the small nerves on the inner side of your heel as these are sometimes trapped by bands of tight tissue. This sort of surgery can be done through a cut about 5cm long on the inner side of your heel. Recently there has been a lot of interest in doing the operation by keyhole surgery, but this has not yet been proven to be effective and safe, and key hole surgery does not allow the nerves to be released.
Most people who have an operation are better afterwards, but it can take months to get the full benefit from the surgery and the wound can take a while to heal fully, for this reason a plaster cast is often used post-operatively.
Surgery is between 70% and 90% successful, however, there are risks, including a
small number of patients who are worse following surgery. The principle complications of surgery include:
- The pain fails to settle
- Dividing the plantar fascia can lead to a flat foot, which is painful, and difficult to treat
- Tingling or numbness in the heel or foot, caused by damage to the small nerves in the heel
- Infection of the wound, slowing down healing
- Excessive bruising
- Swelling of the ankle and foot
In the majority of cases the problems settle, but slow the healing process, occasionally the damage is irreversible. Certainly if you do require surgery your recovery will be helped by keeping your foot up for at least a fortnight after surgery, and following the recovery protocol outlined by the surgical team.
Wouldn’t it be better to take out my heel spur?
As you will have seen from reading the section above ‘I’ve been told my pain is caused by a bone spur’, the pain is not caused by the spur. Rather, both the pain and the spur are caused by inflammation in the plantar fascia. Simple removal of the spur has been known to be ineffective in relieving the pain since the 1960s.
However, if you are one of the rare people who do not respond to simple treatment and end up having an operation to release the plantar fascia, the surgeon may also remove any bone spur at the same time.


