Venous Thromboembolism (VTE) in patients undergoing foot and ankle surgery
Paul Hamilton BMedSci, MBBS, FRCS(T&O)
Andrew “Fred” Robinson BSc, MBBS, FRCS(Orth)
Introduction
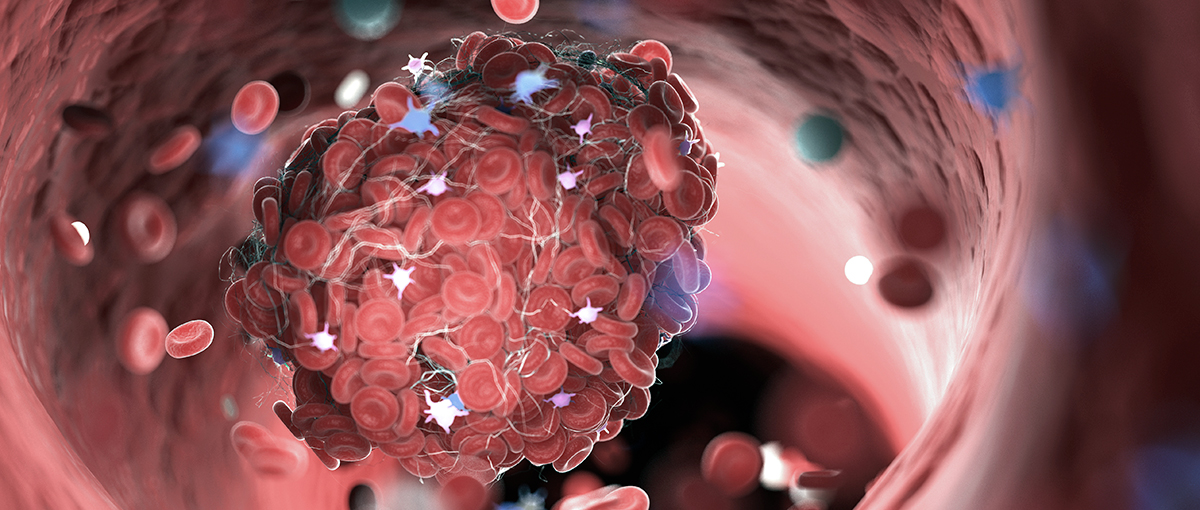
Venous thromboembolism (VTE) is a condition where a blood clot forms in a vein. It most commonly occurs in the leg and is known as a deep vein thrombosis (DVT). In rare circumstances it can dislodge and travel in the blood. This is known as an embolus. If the embolus travels to the lung it is known as a pulmonary embolus (PE).
Why should I be concerned about VTE?
If you develop a DVT, it can dislodge to the lung as a PE. In very rare circumstances a PE can be fatal. Prevention or treatment is therefore very important. In the long term about a quarter of patients who suffer from a DVT develop persistent calf pain and swelling and in the most serious cases ulcers. This is known as post thrombotic syndrome.
What is the risk of VTE in foot and ankle surgery?
The exact risk is unknown but the incidence of DVT is probably less than 1% in patients undergoing foot and ankle surgery. The incidence of PE is substantially less than this, and the risk of a fatal PE is much less than this – we estimate that it is 1 in 5000.
One of the factors determining the risk of VTE is the type of surgery that you undergo. The risk for toe surgery, is minimal. The risk for ankle and hindfoot surgery is also very low. We think that the need for medication to prevent VTE is determined by the factors related to the patient.
The factors related to you – the patient – include smoking, age over 60, varicose veins with inflammation, dehydration, obesity and active cancer. If you have had a VTE in the past, or have a close family member (first degree relative) who has had a VTE you will be at higher risk. If you have any of these risk factors you should inform your doctor.
The oestrogen-containing contraceptive pill and pregnancy increase the risk of VTE. The risk of hormone replacement therapy (HRT) is debatable – in some cases it may be thought safer to stop HRT, in others not.
Your doctor will take into account both the type of surgery and the number of risk factors you have in your assessment. You can develop a VTE even if you have no risk factors.
What are the symptoms of VTE?
Symptoms of DVT include pain, swelling and tenderness of the calf. The leg may also feel heavy and be hot or red. In some circumstances DVT has no symptoms. Symptoms of a PE include chest pain, breathlessness or rarely sudden collapse. If you experience any of these symptoms then you should seek medical advice.
What can I do to reduce the risk of developing VTE?
- Lose weight
- Stop smoking
- Keep well hydrated after surgery – drink lots.
- Stop the oestrogen-containing oral contraceptive pill the cycle before surgery. You will obviously need to use other forms of contraception – this can be discussed with your General Practitioner.
- Consider stopping hormone replacement therapy (HRT) four weeks before surgery
- Perform simple leg exercises when possible – wriggle your toes, bend your hip and knee.
What can we do to reduce the risk of developing VTE?
- Mobilisation – where possible we encourage active mobilisation as soon as possible after surgery
- Anti-embolic stockings – These stocking can be fitted above or below knee. If prescribed they should be used until mobility is resumed, and worn day and night. This is usually for between 4 and 6 weeks. It is important that the stockings are worn correctly as incorrect use can increase the risks of VTE. The stockings should be removed at least once a day for hygiene purposes and to inspect the skin. In the event of pain caused by the stocking or skin damage the use of the stockings should be stopped. Anti-embolic stockings should not be worn if you have reduced circulation or sensation in your legs.
Medication
In some circumstances, when your doctor feels you are at high risk of developing VTE, they may recommend you receive drugs to prevent VTE. The drugs used for prevention of VTE include:
- Low molecular weight heparin (LMWH)
Heparin injections under the skin are the commonest form of VTE prevention used in foot and ankle surgery. These injections reduce the risk of VTE by about 50%. Yourself or a family member can administer the injections. You should be taught how to give the injections before you leave hospital. Occasionally a nurse may have to help you give the injections at home.
With these injections bruising at the site of the injection is relatively common. The injections can also lead to bruising and bleeding at the site of the surgery.
LMWH is of animal origin. If you object to using medication of animal origin please inform your doctor.
- Aspirin
Aspirin alone is not considered adequate protection against VTE. If you are taking aspirin please inform your doctor. In most circumstances aspirin should be stopped seven days prior to surgery – to prevent excessive bleeding. Aspirin can be restarted under the instruction of your doctor. This is usually after you have stopped having the injections. - Warfarin
Warfarin is a blood-thinning agent that is most commonly used for long term treatment of VTE. It is rarely used in the prevention of VTE. This is an oral medication but requires regular blood tests to ensure you are getting the correct dose. If you are taking warfarin you MUST inform your doctor. In most circumstances warfarin should be stopped at least four days before surgery. - Other drugs – Dabigatran and Rivaroxiban.
Currently these drugs are unlicensed in the UK for the use in prevention of VTE for foot and ankle surgery. They are oral medications. Although not available for use currently, they may become available in the future.
If you have any questions regarding this leaflet, VTE or prophylaxis, please feel free to ask your doctor or nurse.