What are flat feet/fallen arches?
Most people have an arch along the inside of the foot. This arch creates a space between the ground and the foot. In many shoes the shoe is designed so that the arch is supported by an “arch support.”
The arch develops in childhood, between the ages of three and 10 years. In some people the arch is minimal or absent, these individuals are said to have “flat feet.” In the majority of cases this “flatness” is NORMAL, and nothing to worry about. Some people have high arches. High arches are associated with problems – although these problems tend to be different to those seen with flat feet. The medical terms for flat foot and high arches are “pes planus” and “pes cavus” respectively.
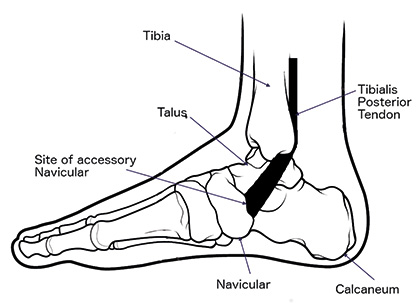
The shape of the bones sets the shape of the foot. The ligaments and muscles form secondary supports. There is a large muscle, the Tibialis Posterior muscle, which supports the arch. Damage to the Tibialis Posterior tendon can cause the foot to flatten.
When Should I worry about my flat foot?
In adults and children you should worry about a flat foot if it is:
- Painful
- Asymmetrical (there is a difference between the two feet)
- The flatness is progressive
- The feet are numb, or you have difficulty feeling them.
In these situations you may choose to seek medical help.
What causes flat feet?
Physiological or Normal Flat Feet:
The vast majority of flat feet fall into this group.
The commonest cause of a flat foot is the so-called “physiological flat foot.” This means that the flatness is a variation of normal. The arch is flattened, but the foot is supple and pain free. When you stand on tiptoes the arch of the foot re-establishes. People with physiologically flat feet often have stretchy ligaments (hypermobility).
If you have physiologically flat feet you can be reassured that there is no structural abnormality needing treatment. Shoes tend to wear out more quickly in people with flat feet, but simply wearing comfortable shoes is the best initial treatment. You should try to buy shoes with an arch support and a well-constructed, supportive heel.
Pathological or Painful Flat Feet:
A small number of people have flat feet, which are a problem. They may require formal treatment. Such feet are said to be “pathological” – which just means abnormal. The causes differ in children and adults.
In children the foot may not develop normally in the womb. The small bones of the foot (tarsals) do not separate properly. The foot is stiff and painful. You may hear your doctors talking about a tarsal coalition – this is just another way of saying that the bones have not separated. You may hear people saying that there is a “bar” – this refers to the abnormal segment of bone, or bar, connecting the bones. Tarsal coalitions, or bars, tend to first be noticed in children or young adults.
The commonest cause of flat foot in adults is stretching of the tibialis posterior tendon, this tendon lifts the arch of the foot. The tendon attaches the tibialis posterior muscle to the navicular bone (see diagram). It runs behind the inner bony prominence (medial malleolus) of your ankle. This tibialis posterior initiates push off as you walk and supports the arch. The tendon works over a very short distance – it only has to move about 1cm. In some people, usually those with a physiological flat foot to start with, the tendon can become worn. With wear the tendon does not usually snap, but stretches. If it stretches more than 1cm it loses all of its effectiveness, and support of the arch is lost. The arch of the foot then flattens.
Occasionally individuals are born with an extra bone (accessory navicular) in the tibialis posterior tendon (see diagram). This extra bone is present in about 10% of people. It is usually pain free, and you may just notice a small prominence over the inside of the arch. The accessory navicular does not need treatment unless it is painful, or “symptomatic.”
A previous fracture of your heel bone can lead to flat feet; the pain from this is due to wear and tear (osteoarthritis) in the joint below the ankle– the subtalar joint. All types of arthritis – including osteo- and rheumatoid arthritis – can cause painful flat feet. Arthritis in the midfoot can lead to a flat foot as well.
What are the symptoms of flat feet?
Often the patient has few symptoms, other than the loss of height of the arch. Nevertheless the stretched tendon on the inside of the ankle can be swollen and painful. As the foot flattens the pain moves to the outside of the ankle, as the tendons are trapped under the fibula and the subtalar joint and the heel tilt. The foot appears turned out.
The pain can be associated with stiffness, and it may be difficult to walk on uneven or cobbled surfaces. The foot looses its side-to-side movement. In very advanced cases the pain can also affect the ankle joint, as at this stage the ankle joint starts to wear unevenly and tilts.
As the arch collapses rough skin (callosities) can develop under the inner border of the foot due to the foot rolling inwards and the arch collapsing. The Achilles tendon or heel cord also tightens.
What sort of assessment do I need?
You should be assessed by an orthopaedic surgeon, ideally one who has trained in foot and ankle surgery. Your assessment will involve you explaining your symptoms and an examination of your lower limbs and your feet.
X-rays are usually required to document the position of the bones in relation to one another, and to assess for joint wear and tear. A magnetic resonance scan (MRI) or an Ultrasound scan (USS) may also be necessary. The MRI can tell if the tendon is swollen, worn or torn; and whether there is joint damage. An ultrasound might show fluid around or a tear of the tendon. MRI and ultrasound studies are not 100% accurate.
If your doctor suspects a generalized disorder, such as arthritis, then you may need blood tests.
Treatment of flat feet
If your flat feet are painless as a result of ligament hyperlaxity surgical treatment is not necessary. If your feet are uncomfortable a supportive insole with an arch support may be helpful. Insoles are also called “orthoses”. It should be noted that insoles do not change the shape of your feet in the long-term. Customised insoles can be very expensive, and it is often better to start by trying shop bought arch supports. Some shoes (for example training shoes) are sold with an arch support in them, alternatively the arch support can be bought independently in a pharmacy.
Flat feet due to tibialis posterior tendon damage
The treatment depends on the severity of the damage to the tendon, as well as the symptoms.
In the early stages when the tendon is simply inflamed, but not stretched out, anti-inflammatory medication, rest, elevation, ice and physiotherapy can be used. Occasionally it will be suggested that the tendon is released with surgery. The foot is rested in either a plaster cast or a removable plastic boot for a period of 4 to 6 weeks.
Once the acute symptoms have settled an insole to support the arch, reducing the amount of work the tendon has to perform, may be recommended.
If the foot is deformed then a corrective insole may be required. This type of insole works best on a mobile deformity; it puts the hindfoot in the correct position for the rest of the foot to function properly. It usually incorporates an arch support with a small wedge underneath the inner aspect of your heel pad. When orthoses are fitted it is important that you have a pair of shoes that will accommodate the foot as well as the orthosis. It can take several months of wearing insoles to find out if they will work.
If you have a deformity that continues to be painful then reconstructive surgery may be considered. Surgery is designed to realign the foot. The operation involves a tendon reconstruction to restore the tendinous support to the arch. The tendon which curls the toes (flexor digitorum longus) is sacrificed for this purpose. You will still be able to curl your toes after surgery. Tendon reconstruction is usually performed through an incision on the inside of your foot. The tendon reconstruction alone is not strong enough in isolation, and a realignment of the heel bone is also performed to recreate the shape of the arch. A separate incision over the heel bone is needed to realign the heel bone.
If you have a stiff hindfoot, which is painful, then a fusion of the foot may be required. This operation stiffens three joints in the back of the foot. This complex of joints lies under the ankle joint and their function is to allow side-to-side movement of the heel, enabling you to walk on uneven ground or across a slope. This option is usually chosen if X-rays show evidence of wear and tear in the joints. The ankle joint will usually be left, and thus you will be able to move your foot up and down, and walk normally, without a limp.
If the heel cord is tight after either tendon reconstruction or triple fusion, then the heel cord is released through a small incision over your calf.
In severely deformed feet where the joints have been totally disrupted and there is dislocation of the joints of the instep, surgical reconstruction may not always be possible. In these cases an insole to protect and cushion the foot can be used to control the symptoms. This option is also useful in patients who are unsuitable or reluctant for surgery. Custom made shoes or boots incorporating insoles is used for these patients.
What to expect after surgery
After surgery, whilst in the operating theatre, your leg will be protected in a half plaster which will stay on the leg for two weeks. At two weeks the sutures are removed and you will be put into a definitive cast, which you can walk on. Every two weeks following surgery your foot will be brought up and out a little and put into a new cast. This will continue for eight weeks until your foot is in a neutral position. This progression is important and avoids overstretching the tendon reconstruction. At eight weeks an X-ray is required to check that the heel bone has united. As long as this has been successful you will be allowed to weight bear out of the cast.
Once you are free from the cast you will be allowed to put more weight on your foot. Physiotherapy may be required to build up the muscles in the leg and to restore the movement to your ankle and hindfoot, which will have become quite stiff in the plaster.
The foot and ankle can remain swollen for up to a year. The reconstruction can take up to a year to develop the strength needed to support the arch again.
After fusion surgery the recovery is very similar, although you will be in a cast for 12, instead of eight weeks. You will be allowed to weight bear after two weeks. At six weeks an X-ray is taken to check if the fusion is healing in the correct position. You will then go back into a cast or pneumatic boot for a further 6 weeks. At 12 weeks the cast will be removed and you will start to build up the muscles in your leg and mobilize the ankle.
Pain control immediately following the operation is achieved through a combination of nerve blocks to numb the leg, and painkillers given as tablets or injections. You will be discharged from the ward once you are safe on crutches and the pain is under control with tablets. You may well be on injections to prevent a blood clot for at least two weeks.
Complications of surgery, and what can go wrong
Generally speaking 95% of patients are satisfied following this type of surgery, although it can take up to 1 year to make a full recovery.
All operations carry certain risks. These include the general risks of surgery and anaesthesia, including deep vein thrombosis, pulmonary embolus (blood clots on the lung) which can sometimes be fatal, problems with the anaesthetic, infection and wound healing problems.
Complications specific to this type of surgery include:
- Failure of the pain to resolve, or worsening of the pain.
- Recurrence of the flattening of the foot, as a result of re-rupture of the reconstructed tendon.
- Stiffness of the ankle and foot.
- Persistent swelling.
- Nerve and blood vessel damage
- Requirement for a second, small operation to remove screws, or plates.
- Failure of the bones to heal together necessitating further surgery.
Smoking increases the risks of surgical failure by five times. This increased complication rate seems to be resultant on nicotine, which is unfortunately found in the patches that are used to assist giving up smoking.


